

East Grampians & Stawell Chronic Disease Integrated Response Initiative
As part of the Western Victoria Primary Health Network (PHN) request for proposals for rural allied health funding, CeRDI was engaged by East Grampians Health Service and Stawell Regional Health to enhance capacity to effectively implement an evidence-based approach for complex health conditions related to place specific issues within the region, as they relate to service delivery.
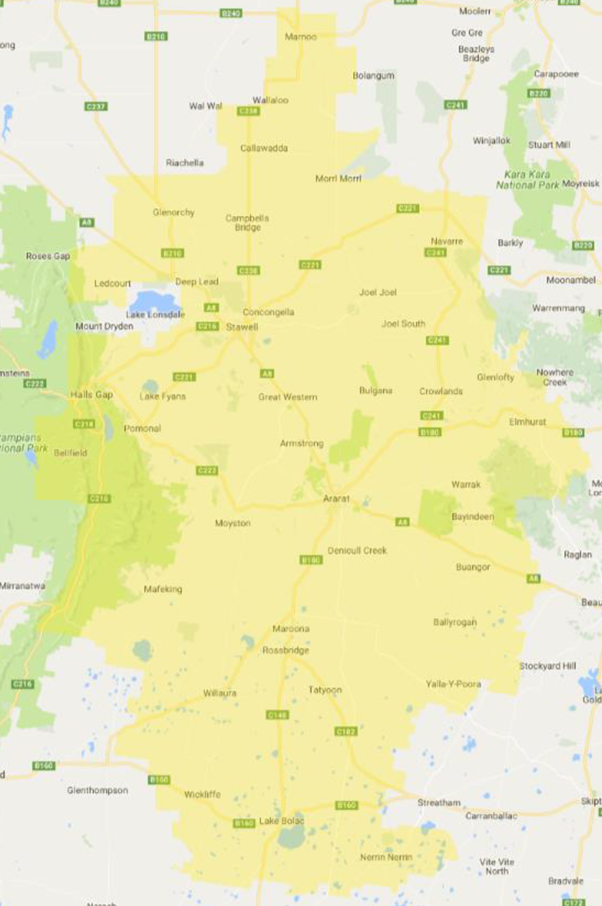 |
| Zone location – where the services will be delivered |
Background
The funding through the Western Victoria Primary Health Network (PHN) provided allied health to rural communities to enable access to those most vulnerable populations. As the prevalence and cost of chronic medical conditions is high within the health system, chronic diseases were the focus of this round of allied health funding which aimed to provide patient centred multidisciplinary care that meets the needs of the local areas and is cost-effective.
The East Grampians and Stawell Chronic Disease Integrated Response Initiative (EGS-CDIRI) is a partnership approach addressing the following conditions:
- Diabetes
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Musculoskeletal
Selection of chronic conditions was based on analysis of priority areas of need, as identified through statistical data for chronic disease across the region.
Wagner’s chronic care model was used as a basis for the service delivery model and recognises elements that are essential for high quality care, including community, the health system, self-management support, delivery system design, decision support and clinical information systems. The model supports evidence-based practice and informed patients that are actively involved in their care.
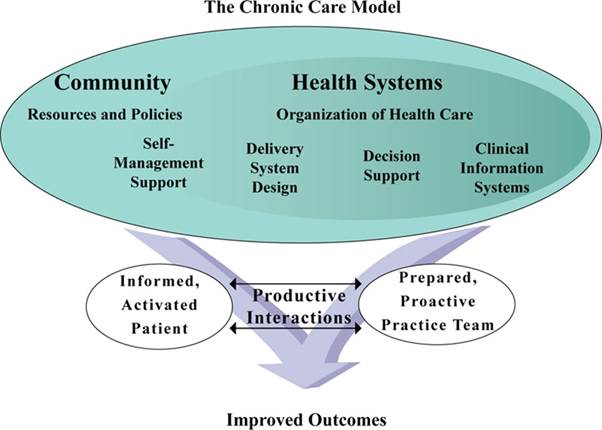 |
| Wagner chronic care model |
To maximise capacity to embed Wagner’s model in service delivery, and to effectively and systemically address the prioritised chronic conditions, a complimentary dual component model has been developed. Component 1 involves a partnership between two health services, targeting structural consolidation and enhancement in the organisation of health care. Component 2 of the model is the captures the specific operational approaches to be used for maximum benefits for patients with identified chronic diseases. The two components, in combination represent the overarching model for this proposal.
The benefits of the model, and the targeted outputs, have been aligned with relevant national standards and evidence-based practice guidelines for addressing the targeted chronic diseases. These relate to:
- Enhanced, embedded, and formalised links with general practice
- Formalised processes for improved care-coordination, case management and shared care
- The establishment of chronic disease management multidisciplinary responses
- Improved coordination/extension of self-management support processes (over patient self-management)
- Increased access to electronic clinical records and enhanced patient management
- Improved understanding and application of evidence-based approaches for chronic disease
- An organisational commitment to professional development, supervision, and support for multidisciplinary practice in chronic disease management
- The facilitation of service access for identified chronic conditions
- A reduction in preventable hospitalisation rates
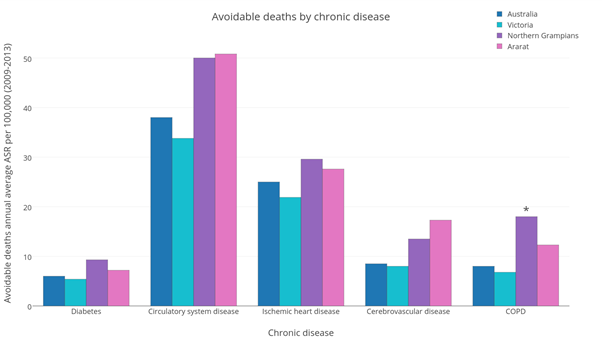 |
| Avoidable deaths annual average ASR per 100,000 by chronic disease |
Outcomes
The request for proposal was successful in securing nearly $1 million in funding for the Stawell and Ararat regions.
Innovation
Innovation in this project is found in the use of a complementary integrated model facilitating:
- Standardisation of health organisation processes across two diverse health services
- Integrated electronic clinical records
- Implementation of MBS (100%) donation across AHP
- Formalised liaison for enhanced service integration with General Practitioners (GPs)
- Health trend tracking through the Wimmera Information Portal
- Localised evidence-based pathways development
- Sharing of staff resources, peer support, networks, and professional development
- The inclusion of a parallel research element to monitor, track and review model implementation against global trends
Approach
- Mapping the evidence base – through stakeholder consultation, community networks, sourcing statistical data, document analysis and literature review
- Developing a service delivery model – using current best practice strategies, responding to identified issues, identifying collaborations, and developing a monitoring mechanism
- Development of the proposal – synthesised the evidence base and delivery model, developed the implementation plan and identified outputs and outcomes for monitoring and review
-
PARTNERS
In collaborative practice with:- Stawell Medical Centre
- Ararat General Practice
- Tristar Medical Group Ararat
- Grampians Community Health
- Buja Buja Aboriginal Cooperative (Halls Gap)
- Rural City of Ararat
- Shire of Northern Grampians
- Ballarat Health Services
- Grampians Pyrenees Primary Care Partnership


